Denials and Appeals
Find the root cause. Address issues. Get paid. Focus on denial prevention.
Denial Management Services
Denial Management Services
What is Denial Management in Healthcare?
Denial management is often confused with Rejection Management. Rejected Claims are claims that have not made it to the payer’s adjudication system on account of errors. The billers must correct and resubmit these claims. Denied Claims, on the other hand, are claims that a payer has adjudicated and denied the payment.
Healthcare organizations should be concerned about both rejected claims and denied claims. The claims rejection management process provides an understanding of the claim’s issues and an opportunity to correct the problems. Denied Claims represent lost revenue or delayed revenue (if the claim gets paid after appeals).
To successfully appeal denied claims, the billers must perform a root-cause analysis, take actions to correct the identifies issues, and file an appeal with the payer. To thrive, a healthcare organization must continuously address the front-end processes’ problems to prevent denials from recurring in the future.
What is Denial Management in Healthcare?
Denial management is often confused with Rejection Management. Rejected Claims are claims that have not made it to the payer’s adjudication system on account of errors. The billers must correct and resubmit these claims. Denied Claims, on the other hand, are claims that a payer has adjudicated and denied the payment.
Healthcare organizations should be concerned about both rejected claims and denied claims. The claims rejection management process provides an understanding of the claim’s issues and an opportunity to correct the problems. Denied Claims represent lost revenue or delayed revenue (if the claim gets paid after appeals).
To successfully appeal denied claims, the billers must perform a root-cause analysis, take actions to correct the identifies issues, and file an appeal with the payer. To thrive, a healthcare organization must continuously address the front-end processes’ problems to prevent denials from recurring in the future.
Our Denial Management Service Offering
- Investigate the reason for every denied claim
- Focus on resolving the issue
- Resubmit the request to the insurance company
- File appeals where required
Medical Billing Wholesalers’ denial management team has seasoned professionals who:
We understand that each denial case is unique. We correct invalid or incorrect medical codes, provide supporting clinical documentation, appeal any prior authorization denials, understand any genuine denial cases to pass the responsibility to patients, and follow-up effectively. We re-validate all clinical information before re-submission.
As an extended billing office, we work with you to analyze your denied claims and reduce denial % over time.
Filing Appeals
We analyze denial reasons, prepare appeal letters, and refile the claims by attaching clinical documentation and submit the claims via fax appeals in a payer-specific format.
Reducing Denials Through Analytics
Different component processes within the revenue cycle chain can result in claim denials. Often, denial issues are practice-specific or facility-specific. We understand the trends in claim denials and launch an iterative process to reduce them based on specific causes.
Client Testimonials
Texas based HealthCare Centre
“I wanted to thank the Medical Billing Wholesalers team for providing us assistance with our address change project. They are very responsive, attentive and proactive in resolving our concerns. Thanks to the MBW management for providing us amazing people to help at critical times in our practice evolution process-which I sincerely appreciate!”
Get the White paper
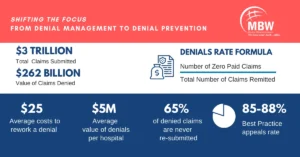
Denial Management Infographic
Ready to take your business to the next level?
Get in touch today and receive a complimentary consultation.
Our users are Happy & Healthy
“I want to take a moment to thank Medical Billing Wholesalers for their extra hard work and commitment in reducing our Missing Slip inventory. The combined efforts of Offshore and our TVH Team had our Missing Slip Inventory down from 22K to 13K.”
Florida based Healthcare Centre
“I want to take a moment to thank Medical Billing Wholesalers for their extra hard work and commitment in reducing our Missing Slip inventory. The combined efforts of Offshore and our TVH Team had our Missing Slip Inventory down from 22K to 13K.”
Florida based Healthcare Centre
“I want to take a moment to thank Medical Billing Wholesalers for their extra hard work and commitment in reducing our Missing Slip inventory. The combined efforts of Offshore and our TVH Team had our Missing Slip Inventory down from 22K to 13K.”
Florida based Healthcare Centre
Healthcare partnerships

Effectively Combat Clinical Denials and Shift Focus to Denial Prevention
Benefits of Our Clinical Denial Management Services
Improved Revenue Recovery:
Our Denial Management Services are at the forefront of recovering revenue from denied claims. We diligently work to identify, address, and appeal claim denials, significantly boosting your revenue recovery rates.
Reduction in Claim Denials
By thoroughly analyzing the reasons behind claim denials, we help in refining your billing practices. This proactive approach not only reduces future denials but also minimizes revenue loss and streamlines your billing processes.
Enhanced Operational Efficiency
Embrace efficiency with our services. We automate and optimize various tasks within the revenue cycle, minimizing manual errors and maximizing operational productivity.
Data-Driven Insights for Better Decision-Making
Our approach is grounded in analytics. By examining denial patterns, we provide actionable insights that help in making informed decisions, improving your overall billing strategy.
Significant Cost Savings >50%
By partnering with us, you’re not just improving your revenue cycle efficiency; you’re also choosing a cost-effective solution. Our Denial Management Services lead to significant cost savings by reducing denials and optimizing your overall revenue cycle.
Compliance and Regulatory Assurance
Navigating the complexities of healthcare regulations can be daunting. Our services ensure that your claims are compliant with current regulations, reducing the risk of penalties and ensuring adherence to industry standards.
Explore our Latest Thinking
Contact Us for ABA Therapy Billing Services
Contact us today to learn more about our ABA Therapy Billing Services and how we can help your practice optimize its revenue cycle.